Chapter 2: Reproduction in Lower and Higher Animals
Multiple choice question.
The number of nuclei present in a zygote is _______.
two
one
four
eight
Which of these is the male reproductive organ in humans?
sperm
seminal fluid
testes
ovary
Attachment of embryo to the wall of the uterus is known as _______.
fertilization
gestation
cleavage
implantation
Rupturing of follicles and discharge of ova is known as _______.
capacitation
gestation
ovulation
copulation
In human female, the fertilized egg gets implanted in uterus _______.
After about 7 days of fertilization
After about 30 days of fertilization
After about two months of fertilization
After about 3 weeks of fertilization
Test tube baby technique is called _______.
in vivo fertilization
in situ fertilization
in vitro fertilization
artificial insemination
The given figure shows human sperm. Various parts of it are labelled as A, B, C, and D. Which labelled part represents acrosome?
B
C
D
A
Presence of beard in boys is a _______.
primary sex organ
secondary sexual character
secondary sex organ
primary sexual character
Answer in one sentence.
What is the difference between a foetus and an embryo?
Answer:
The embryo is the developing organism from fertilization to the end of the eighth week of development. It develops into the foetus.
The foetus is the developing organism from the beginning of the third month to birth.
Outline the path of sperm upto the urethra.
Answer:
Seminiferous tubules → Rete testis → Vasa efferentia → Epididymis → Vas deferens → Ejaculatory duct → Urethra
Which glands contribute fluids to the semen?
Answer:
The seminal vesicle, prostate gland and Cowper’s / Bulbourethral gland contribute fluids to the semen.
Name the endocrine glands involved in maintaining the sex characteristics of males.
Answer:
Testes (gonads)
Where does fertilization and implantation occur?
Answer:
Fertilization usually takes place in the ampulla of the fallopian/uterine tube, while implantation occurs in the endometrium of the uterus.
Enlist the external genital organs in the female.
Answer:
The external genital organs of female include parts external to the vagina, collectively called vulva (covering or wrapping), or pudendum. They include the following parts:
Vestibule:
It is a median vertical depression of the vulva enclosing the urethral and vaginal opening.
Labia minora:
These are another pair of thin folds inner to the labia majora with which they merge posteriorly to form the fourchette (frenulum), while towards the anterior end they converge into a hood-like covering around the clitoris.
Clitoris:
A small conical and sensitive projection lying at the anterior end of labia minora. It has a pair of erectile tissue i.e. corpora cavernosa which is homologous to the penis.
Labia majora:
These are a pair of fleshy folds of skin forming the boundary of the vulva. They are homologous to the scrotum. They surround and protect the other parts of the external genitalia and enclose the urethral and vaginal openings in the vestibule.
Mons pubis:
It is a fleshy elevation above the labia majora. The Mons pubis and outer part of labia majora show pubic hair.
Give two differences between blastula and gastrula.
Answer:
What is the difference between embryo and zygote?
Answer:
Fill in the blank:
The primary sex organ in human male is _______.
Answer:
The primary sex organ in human male is the testis.
The _______ is also called the womb.
Answer:
The uterus is also called the womb.
Sperm fertilizes ovum in the _______of fallopian tube.
Answer:
Sperm fertilizes ovum in the ampulla of fallopian tube.
The disc-like structure which helps in the transfer of substances to and from the fetus’s body is called _______.
Answer:
The disc-like structure which helps in the transfer of substances to and from the fetus’s body is called placenta.
Gonorrhoea is caused by _______ bacteria.
Answer:
Gonorrhoea is caused by Neisseria gonorrhoeae bacteria.
The hormone produced by the testis is _______.
Answer:
The hormone produced by the testis is testosterone.
Short answer question.
Write a note on budding in Hydra.
Answer:
1. Asexual reproduction in Hydra takes place through budding.
2. Budding normally occurs in favorable conditions.
3. In Hydra, a small outgrowth is produced towards the basal end of the body.
4. It develops as a bud which grows and forms tentacles.
5. This bud eventually develops (get transformed) into a new individual.
6. The young Hydra gets detached from the parent and becomes an independent new organism.
Budding in Hydra-
Explain the different methods of reproduction occurring in sponges.
Answer:
Asexual reproduction in sponges:
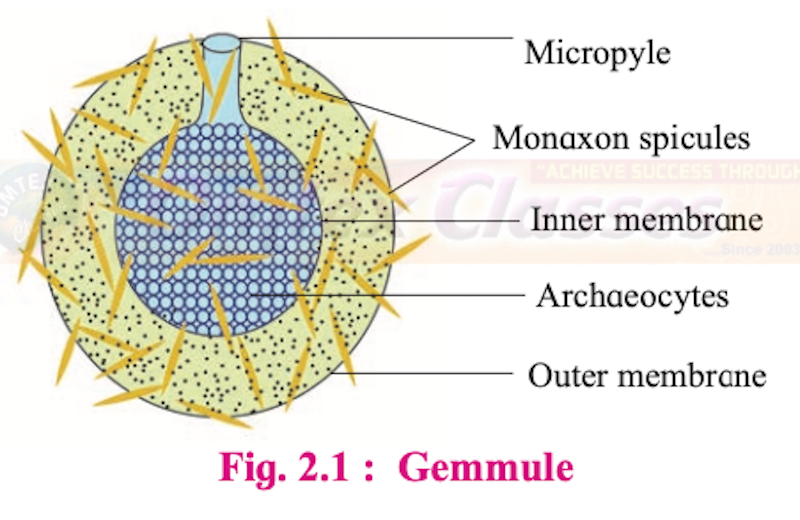
1. Sponges reproduce asexually via. gemmule formation. Gemmule is an internal bud formed only in sponges to overcome unfavorable conditions.
2. The structure of the gemmule includes the micropyle, spicule, inner layer, archaeocytes, and outer layer.
3. It possesses an asexually produced mass or aggregation of dormant cells known as archaeocytes. These cells are capable of developing into a new organism (totipotent).
4. The archaeocytes get coated by a thick resistant layer of secretion by amoebocytes.
5. Monaxon spicules (developed by growth along a single axis) are secreted by scleroblasts in between the inner and outer membrane.
6. On return of favorable conditions of water and temperature, the gemmules hatch and develop into a new individual.
7. There is a minute opening called micropyle through which the cells (new individuals) come out during favourable conditions.
Sexual reproduction in sponges:
1. Poriferans that reproduce by the sexual method are hermaphrodites and produce sperms and eggs at different times.
2. Sperms disseminated into the water column, are subsequently captured by female sponges of the same species.
3. Inside the female, the sperm is transported to eggs by means of archaeocytes.
4. Fertilization occurs and zygotes develop into ciliated larvae.
5. Once these larvae are in the water column, they settle and develop into juvenile sponges.
Write a note on IVF.
Answer:
IVF (In-vitro Fertilization):
It is a process of fertilization where an egg is combined with sperm outside the body in a test tube or glass plate to form a zygote under simulated conditions in the laboratory. The zygote or early embryos (with up to 8 blastomeres) could be then transferred into the fallopian tube for further development.
Comment on any two mechanical contraceptive methods.
Answer:
Mechanical means / Barrier methods:
In this method, the ovum and sperm are prevented from physically meeting with the help of barriers. These mechanical barriers are of three types.:
1. Condom:
It is a thin rubber sheath that is used to cover the penis of the male during copulation.
It prevents the entry of ejaculated semen into the female reproductive tract. It can thus prevent conception. It is a simple and effective method and has no side effects.
Condoms should be properly discarded after every use.
Condom is also a safeguard against STDs and AIDS.
e.g. “Nirodh” is the most widely used contraceptive by males. It is easily available and is given free by the government.
2. Diaphragm, cervical caps and vaults:
These devices used by the female are made up of rubber. They prevent conception by blocking the entry of sperms through the cervix. The device is inserted into the female reproductive tract to cover the cervix during copulation.
3. Intra-uterine devices (IUDs):
These clinical devices are plastic or metal objects. A doctor or trained nurse places the IUDs into the uterus. These devices include Lippes loop, copper releasing IUDs (Cu-T, Cu7, multiload 375), and hormone-releasing IUDs (LNG-20, progestasert).
i. Lippes loop:
It is a plastic double “s” loop. It attracts the macrophages stimulating them to accumulate in the uterine cavity. Macrophages increase phagocytosis of sperms within the uterus and act as a contraceptive.
ii. Copper releasing IUDs:
Suppress sperm motility and the fertilizing capacity of sperms.
iii. Hormone releasing IUDs:
Make the uterus unsuitable for implantation and the cervix hostile to the sperms. It delays pregnancy for a longer period.
Drawbacks: Spontaneous expulsion, occasional haemorrhage, and chances of infection are the drawbacks of IUDs.
Write a note on tubectomy.
Answer:
1. Tubectomy is a permanent birth control method in women.
2. It is performed by removing a small part of the fallopian tube or tying it up through a small incision in the abdomen or through the vagina.
3. These techniques are highly effective but their reversibility is highly poor.
4. Sometimes it becomes necessary to use these methods either to prevent pregnancy or to delay or space pregnancy due to personal reasons.
5. This method blocks gamete transport and prevents pregnancy.
Give the name of the causal organism of syphilis and write on its symptoms.
Answer:
1. Causative agent:
Treponema pallidum (Bacteria)
2. Symptoms:
Primary lesion called chancre at the site of infection. The chancre is formed on the external genitalia, skin rashes, and mild fever, inflamed joints, loss of hair. Paralysis, Degenerative changes occur in the heart and brain.
What is colostrum?
Answer:
1. Colostrum is sticky and yellow fluid secreted by the mammary glands soon after childbirth.
2. It contains proteins, lactose, and mother’s antibodies e.g. IgA.
3. The fat content in colostrum is low.
4. The antibodies present in it helps in developing resistance for the new born baby at a time when its own immune response is not fully developed.
Answer the following question.
Describe the phases of the menstrual cycle and their hormonal control.
Answer:
The menstrual cycle involves a series of cyclic changes in the ovary and the female reproductive tract, mainly in the uterus.
It is divided into four phases:
i. Menstrual phase
ii. Proliferative phase
iii. Ovulatory phase
iv. Secretory phase or luteal phase
i. Menstrual phase:
The beginning of each cycle is taken as the first day when menses or loss of blood takes place. During this phase, about 45-100ml of blood is lost.
This phase lasts for approximately five days (average 3-7 days).
The blood in the menstrual discharge does not clot due to the presence of fibrinolysin.
Menstrual phase occurs when an ovulated egg does not get fertilized and it is thereby shed out along with the menstruum. This process is also referred to as the ‘funeral of unfertilized egg’.
Changes in the uterus:
The endometrium of the uterus breaks down under the effect of prostaglandins released due to decreased levels of progesterone and estrogen.
During menses, the blood, tissue fluid, mucus, endometrial lining, and the unfertilized oocyte is discharged through the vagina. Also, the endometrial lining becomes very thin i.e. about 1 mm.
Changes in the ovary:
During these five days, many primordial follicles develop into primary and few of them into secondary follicles under the effect of FSH.
ii. Proliferative phase / Follicular phase / Post menstrual phase:
This phase is the duration between the end of menstruation and the release of ovum (ovulation). The duration of this phase is more variable than other phases. Generally, it extends from 5th to 13th day of the menstrual cycle.
Changes in the ovary:
Generally, out of 6 to 12 secondary follicles that proceed to develop, only one develops into a Graafian follicle (mature follicle). while the rest of the follicles degenerate (atresia). The stimulation for proliferation of new follicles is influenced by GnRH which stimulates release of FSH. The developing secondary follicles secrete the hormone estrogen.
Changes in the uterus:
Endometrium begins to regenerate under the effect of gradually increasing the number of estrogens. Regeneration also involves the formation of endothelial cells, endometrial or uterine glands, and network of blood vessels. The thickness of the endometrium reaches 3-5 mm.
iii. Ovulatory phase:
It is the shortest phase of menstrual cycle.
Changes in the ovary:
It involves rupturing of the mature Graafian follicle and release of an ovum (secondary oocyte) into the pelvic cavity; usually on 14th day of the menstrual cycle. Rapid secretion of LH by a positive feedback mechanism causes the mature follicle to rupture. Ovulation may be accompanied by mild or severe pains in lower abdomen.
iv. Secretory phase / Luteal phase:
It is the phase between ovulation and the beginning of the next menses. This phase is the longest phase. It lasts for 14 days i.e., from 15th to 28th day of the cycle.
Changes in the ovary:
After release of secondary oocyte, remaining tissue of Graafian follicle transforms into a corpus luteum under the effect of LH. The corpus luteum releases progesterone, small amount of estrogen, and inhibin.
The ovulated egg may get fertilized within 24 hours. In the absence of fertilization: the Corpus luteum can survive for only two weeks and then degenerates into a white scar called corpus albicans. In case of fertilization: The embryo is implanted, there is a secretion of human chorionic gonadotropin (hCG), which extends the life of corpus luteum and stimulates its secretory activity. The presence of hCG in maternal blood and urine is an indicator of pregnancy. In absence of fertilization, the next menstrual cycle begins.
Changes in the uterus:
Under the influence of progesterone and estrogen, the endometrial glands grow, become coiled, and start uterine secretions. Endometrium becomes more vascularized and thickens up to 8-10 mm. Inhibin stops secretion of FSH. These changes are necessary for fertilization and subsequent implantation.
Explain the steps of parturition.
Answer:
Parturition is the process of giving birth to a baby. The physical activities involved in parturition like uterine and abdominal contractions, dilation of the cervix, and passage of baby are collectively called labour. Labour is accompanied by a localised sensation of discomfort or agony called labor pains. Parturition involves the following three steps:
1. Dilation stage:
Uterine contractions begin from the top, forcing the baby towards the cervix. Contractions are accompanied by pain caused by compression of blood vessels. Oxytocin induces uterine contractions which become stronger and stronger due to stimulatory reflex. As the baby is pushed down in the uterus, its head comes to lie against the cervix. The cervix gets dilated and the vagina also shows similar dilation. This stage of labour can normally last up to few hours. It ends in the rupturing of amniotic sac of the foetus.
2. Expulsion stage:
During this stage, the uterine and abdominal contractions become stronger. In normal delivery, the fetus passes out through the cervix and vagina with head in the forward direction. It takes around 20 to 60 minutes. The umbilical cord is tied and cut off close to the baby’s navel.
3. After birth:
After the delivery of the baby, the placenta separates from the uterus and is expelled out as “after birth”, due to severe contractions of the uterus. This process happens within 10 to 45 minutes of delivery.
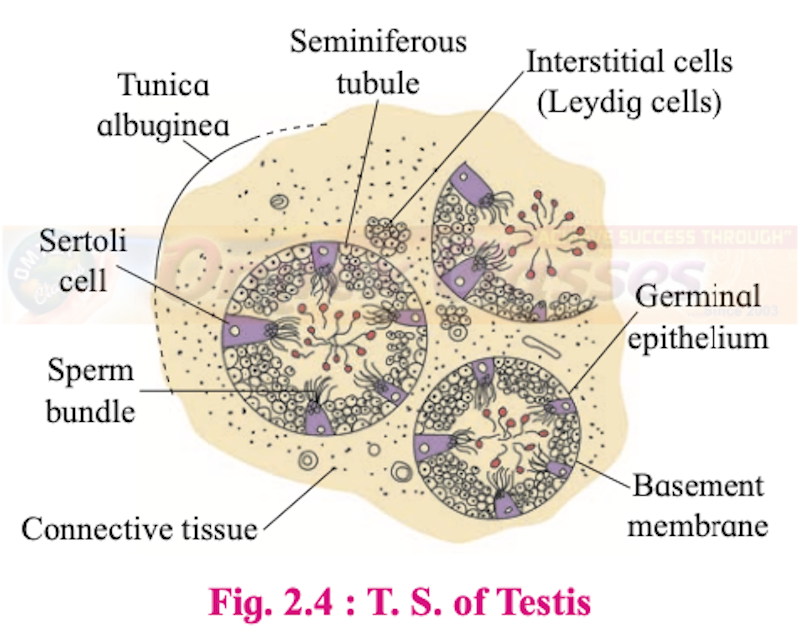
Explain the histological structure of testis.
Histology of Testis:
1. Externally, the testis is covered by three layers. These are:
a. Tunica vaginalis: It is the outermost incomplete peritoneal covering made up of connective tissue and epithelium.
b. Tunica albuginea: It is the middle layer formed by collagenous connective tissue.
c. Tunica vasculosa/vascularis: It is the innermost layers. It is a thin and membranous layer.
2. Each testis is divided into about 200-300 testicular lobules by fibres from tunica albuginea. Each lobule has 1 to 4 highly coiled seminiferous tubules.
3. Each seminiferous tubule is internally lined by a single layer of cuboidal germinal epithelial cells (spermatogonia) and few large pyramidal cells called Sertoli or sustentacular cells.
4. The germinal epithelial cells undergo gametogenesis to form spermatozoa.
5. Sertoli cells provide nutrition to the developing sperms.
6. Various stages of spermatogenesis can be seen in the seminiferous tubules. The innermost spermatogonial cell (2n), primary spermatocyte (2n), secondary spermatocyte (n), spermatids (n) and sperms (n).
7. Between seminiferous tubules, few groups of interstitial cells (Cells of Leydig) are present
8. After puberty, interstitial cells produce a type of androgen i.e. testosterone.
Describe the structure of blastula.
Answer:
Blastulation is the process of formation of the hollow and multicellular blastocyst. The process of blastulation can be summarized as follows:
1. The embryo (blastocyst) that enters the uterus remains floating in uterine cavity for 2-4 days after its entry i.e. till the end of 7th day after fertilization.
2. The outer layer of cells seen in the morula now forms the layer called the trophoblast.
3. Cells from the trophoblast begin to absorb the glycogen rich uterine milk
4. The blastocyst doubles in size from 0.15 mm to 0.30 mm.
5. With more fluid entering inside the blastocyst cavity is formed.
6. These outer cells become flat and are called trophoblast cells (since they help only in absorbing nutrition for the developing embryo).
7. The larger inner cells form inner cell mass or embryoblast (the embryo proper develops from the embryoblasts).
8. These remain attached to the trophoblasts on only one side.
9. The trophoblast cells in contact with the embryonal knob are called cells of Rauber.
10. At this stage, the blastocyst shows polarity i.e. the side with inner cell mass is called the embryonal end and the side opposite to it is the abembryonic end.
11. By the end of the 7th day the blastocyst is fully formed and ready for implantation and gastrulation.
12. The function of zona pellucida is to prevent the implantation of the embryo at an abnormal site. It does not expose the sticky and phagocytic trophoblast cells till it reaches the implantation site i.e. within the uterus, after which the zona pellucida ruptures.
Explain the histological structure of ovary in human.
Answer:
Histological structure of ovary:
Each ovary is a compact structure differentiated into a central part called medulla and the outer part called the cortex. The cortex is covered externally by a layer of germinal epithelium. The stroma of loose connective tissue of the medulla has blood vessels, lymph vessels, and nerve fibers.
The outer cortex is more compact and granular.
It shows large number of tiny masses of cells called ovarian follicles. These are collectively formed from the immature ova originating from cells of the dorsal endoderm of the yolk sac. The cells migrate to the gonadal ridge during embryonic development and divide mitotically.
Now these cells are called oogonia.
As the oogonia continue to grow in size they are surrounded by a layer of granulosa cells. This assembly forms the rudiments of the ovarian follicles. The process of oogenesis starts much before the birth of the female baby and by the end of twelve weeks the ovary is fully formed. The ovary has more than two million primordial follicles in it. The cells of the germinal epithelium give rise to groups of oogonia projecting into the cortex in the form of cords called egg tubes of Pfluger. Each cord at its end has a round mass of oogonial cells called egg nests, from which the primordial ovarian follicles develop. Each primordial follicle has, at its center a large primary oocyte (2n) surrounded by a single layer of flat follicular cells. The primary oocyte starts with its meiotic division but gets arrested it at meiosis I.
Of the two million primordial follicles embedded in the fetal ovary only about one million remains at birth and only about 40,000 remain at the time of puberty.
T.S. of Ovary-
The histological structure of the ovary shows the different stages of development of the oocyte in the ovary. These changes are cyclic and occur during each menstrual cycle. This development involves maturation of the primordial follicles into primary, secondary and Graafian follicles.
Each primary follicle has multi-layered cuboidal follicular cells. The stroma cells add theca over the follicle, which then changes into a secondary follicle.
There is the growth of the oocyte and the granulosa cells increase in number. They start producing the hormone estrogen.
The secondary follicle grows into the Graafian follicle by the addition of more follicular cells.
As this process of maturation of follicles takes place, they begin to move towards the surface of the ovary. The Graafian follicle presses against the thin wall of the ovary giving it a blistered appearance.
The egg is released from the Graafian follicle during ovulation and the remaining part of the follicle changes into a temporary endocrine gland called corpus luteum.
If fertilization does not take place the corpus luteum degenerates into a white scar called corpus albicans.
Describe the various methods of birth control to avoid pregnancy.
Answer:
Contraceptive methods are of two main types i.e. temporary and permanent.
1. Temporary methods:
i. Natural method/ Safe period / Rhythm method:
In the natural method, the principle of avoiding chances of fertilization is used. A week before and a week after menstrual bleeding is considered a safe period for sexual intercourse.
This method is based on the fact that ovulation occurs on the 14th day of the menstrual cycle. Drawback: High rate of failure.
ii. Coitus Interruptus or withdrawal:
In this method, the male partner withdraws his penis from the vagina just before ejaculation, so as to avoid insemination.
Drawback: Pre-ejaculation fluid may contain sperms and this can cause fertilization.
iii. Lactational amenorrhea (absence of menstruation):
This method is based on the fact that ovulation does not occur during the period of intense lactation following parturition. Therefore, as long as the mother breastfeeds the child fully, chances of conception are almost negligible.
Drawbacks: High chances of failure.
iv. Chemical means (spermicides):
In this method, chemicals like foam, tablets, jellies, and creams are used by the female partner. Before sexual intercourse, if these chemicals are introduced into the vagina, they adhere to the mucous membrane, immobilize and kill the sperms.
Drawback: It may cause allergic reaction. This method also has chances of failure.
v. Mechanical means / Barrier methods:
In this method, the ovum and sperm are prevented from physically meeting with the help of barriers.
These mechanical barriers are of three types.:
1. Condom:
It is a thin rubber sheath that is used to cover the penis of the male during copulation. It prevents the entry of ejaculated semen into the female reproductive tract. It can thus prevent conception. It is a simple and effective method and has no side effects. Condoms should be properly discarded after every use. A condom is also a safeguard against STDs and AIDS.
e.g.“Nirodh” is the most widely used contraceptive by males. It is easily available and is given free by the government.
2. Diaphragm, cervical caps and vaults:
These devices used by the female are made up of rubber. They prevent conception by blocking the entry of sperms through the cervix. The device is inserted into the female reproductive tract to cover the cervix during copulation.
3. Intra-uterine devices (IUDs):
These clinical devices are plastic or metal objects. A doctor or trained nurse places the IUDs into the uterus. These devices include the Lippes loop, copper releasing IUDs (Cu-T, Cu7, multiload 375), and hormone-releasing IUDs (LNG-20, progestasert).
Lippes loop:
It is a plastic double “s” loop. It attracts the macrophages stimulating them to accumulate in the uterine cavity. Macrophages increase phagocytosis of sperms within the uterus and act as a contraceptive.
Copper releasing IUDs:
Suppress sperm motility and the fertilizing capacity of sperms.
Hormone releasing IUDs:
Make the uterus unsuitable for implantation and cervix hostile to the sperms. It delays pregnancy for a longer period.
Drawbacks: Spontaneous expulsion, occasional haemorrhage and chances of infection are the drawbacks of IUDs.
vi. Physiological (Oral) Devices:
Physiological devices are used in the form of tablets/ pills. It is an oral contraceptive, used by the female which contains progesterone and estrogen. These hormones inhibit ovulation; hence no eggs are released from the ovary of the female using this pill and thus conception cannot occur.
They also alter the quality of cervical mucus to prevent the entry of sperms. The pill “Saheli” is an oral contraceptive for females which is non-steroidal. Saheli is to be taken once in a week. These pills are sponsored by the Government. Saheli is now a part of the National Family Programme as an oral contraceptive pill in India.
Drawback: Oral contraceptive pills have side effects such as nausea, weight gain, tenderness of breast, and slight blood loss between menstrual periods.
vii. Other contraceptives:
The birth control implant is a contraceptive used by the female. e.g. implanon, explanon, etc. It is a tiny, thin rod about the size of a matchstick. It is implanted under the skin of the upper arm and contains progesterone and estrogen. Their mode of action is similar to that of pills. They prevent pregnancy for 3-4 years.
2. Permanent Methods:
The permanent birth control method in men is called vasectomy and in women it is called tubectomy. These are surgical methods, also called sterilization. In vasectomy a small part of the vas deferens is tied and cut. In tubectomy, a small part of the fallopian tube is tied and cut. This blocks gamete transport and prevent pregnancy.
What are the goals of RCH programme.
Answer:
The goals of the Reproductive and Child Healthcare (RCH) programme are as follows:
i. To create awareness among people about various aspects related to reproduction.
ii. To provide facilities to people in order to understand and build up reproductive health.
iii. To provide support for building up a reproductively healthy society.
iv. To bring about a change mainly in three critical health indicators i.e. reducing total infertility rate, infant mortality rate, and maternal mortality rate.
Which hormones are involved in parturition?
Answer:
Parturition is controlled by a complex neuroendocrine mechanism.
1. Signals arise from the fully formed foetus and placenta cause mild uterine contractions.
2. This is accompanied by rise in estrogen- progesterone ratio, increase in oxytocin receptors in uterine muscles.
3. Increase in hormone ratio causes vigorous contractions of myometrium of uterus at the end of pregnancy.
4. The fully developed foetus gives signals for the uterine contractions by secreting Adrenocorticotropic Hormone (ACTH) from pituitary and corticosteroid from adrenal gland.
5. This, in turn, triggers the release of oxytocin from mother’s pituitary gland, which acts on the uterine muscles of the mother and causes vigorous uterine contractions leading to the expulsion of the baby from the uterus.
Which is the function of male accessory glands?
Answer:
Male accessory glands secrete substances that protect the gametes and facilitate their movement.
1. Seminal vesicles:
These are a pair of small fibromuscular pouches present on the posterior side of the urinary bladder. They secrete a seminal fluid (alkaline) containing citric acid, fructose, fibrinogen and prostaglandins. About 60% of the total volume of semen is made up of seminal fluid.
Fructose provides energy to sperms for swimming, while fibrinogen helps in coagulation of semen after ejaculation for quick propulsion into the vagina. The prostaglandins stimulate reverse peristalsis in the vagina and uterus aiding the faster movement of sperms towards the egg in the female body.
2. Prostate gland:
The prostate gland consists of 20 to 30 lobes and is located under the urinary bladder. It surrounds the urethra. It releases a milky white, alkaline fluid called prostatic fluid into the urethra. Prostatic fluid forms about 30% of the total volume of semen. It contains citric acid, acid phosphatase, and various other enzymes.
The acid phosphatase protects the sperm from the acidic environment of the vagina.
3. Cowper’s glands:
Cowper’s glands are also known as bulbourethral glands. These are pea-sized and lie on either side of membranous urethra. They secrete a viscous, alkaline, mucous like fluid which acts as a lubricant during copulation.
Semen: It is the viscous, alkaline and milky fluid (pH 7.2 to 7.7) ejaculated by the male reproductive system.
Generally, 2.5 to 4.0 ml of semen is given out during a single ejaculation and it contains about 400 million sperms.
Semen contains secretion of the epididymis and the accessory glands for nourishing (fructose), neutralizing acidity (Ca++, bicarbonates), activation for movement (prostaglandins).
What is capacitation? Give its importance.
Answer:
Capacitation generally requires 5-6 hours during which the acrosome membrane becomes thin, Ca++ enters the sperm, and sperm tails begin to show rapid whiplash movements.
As a result of capacitation, sperms become extra active and begin to start moving upwards from the vagina to the uterus and to the oviducts. Prostaglandins activate the sperms. The vestibular secretions of the female also enhance sperm's motility. The sperms swim at an average speed of 1.5 to 3.0 mm/min and reach the ampulla. The contraction of uterus and fallopian tubes stimulated by oxytocin of females also aids in the movement of sperm. After capacitation the sperms may reach the ampulla within 5 minutes.
Explain the following parts of male reproductive system along with labelled diagram showing these parts- Testis, vasa deferentia, epididymis, seminal vesicle, prostate gland and penis.
The male reproductive system consists of the following:
i. Primary sex organs (Gonads): Testes
ii. Accessory organs: Accessory ducts and accessory glands
iii. External genitalia: Scrotum and Penis
i. Primary sex organs: Testes
Testes are a pair of primary sex organs which are mesodermal in origin. They are located outside the abdomen in a pouch called scrotum, i.e. extra-abdominal in position. Testes develop in the abdominal cavity (early foetal life) and later descend into the scrotal sac through a passage called inguinal canal. They are suspended in the scrotal sac by the spermatic cord. Testes are connected to the wall of scrotum by a short fibromuscular band called gubernaculum.
They are oval in shape, about 4 to 5 cm long, 2 to 3 cm wide, and 3 cm thick.
The outermost covering of the testis is formed of a dense fibrous membrane called tunica albuginea.
ii. Accessory sex organs:
It includes accessory ducts, accessory glands.
a. Accessory ducts:
1. Rete testis:
The seminiferous tubules of the testis at the posterior surface form a network of tubules called rete testis. The rete testis opens into vasa efferentia.
2. Vasa efferentia:
Vasa efferentia are 12-20 fine tubules arising from the rete testis and join to the epididymis. They carry sperms from the testis and open into the epididymis.
3. Epididymis:
It is a long and highly coiled tube which is differentiated into an upper caput-, middle corpus- and lower cauda epididymis. The sperms undergo maturation in the epididymis.
4. Vasa deferens:
The vas deferens travels up to the abdominal cavity and loops over the ureter to open into the urethra. Vas deferens join the seminal vesicle to form ejaculatory duct.
5. Ejaculatory ducts:
The ejaculatory duct passes through the prostate gland and opens into the urethra.
6. Urethra:
The urethra provides a common passage for the urine and semen and hence is also called urinogenital duct. In males the urethra is long and extends through the penis. It opens to the outside by an opening called the urethral meatus or urethral orifice.
b. Accessory glands:
1. Seminal vesicles:
These are a pair of small fibromuscular pouches present on the posterior side of the urinary bladder. They secrete a seminal fluid (alkaline) containing citric acid, fructose, fibrinogen, and prostaglandins. About 60% of the total volume of semen is made up of seminal fluid. Fructose provides energy to sperms for swimming, while fibrinogen helps in coagulation of semen after ejaculation for quick propulsion into the vagina. The prostaglandins stimulate reverse peristalsis in vagina and uterus aiding the faster movement of sperms towards the egg in the female body.
2. Prostate gland:
Prostate gland consists of 20 to 30 lobes and is located under the urinary bladder. It surrounds the urethra. It releases a milky white, alkaline fluid called prostatic fluid into the urethra. Prostatic fluid forms about 30% of the total volume of semen. It contains citric acid, acid phosphatase and various other enzymes.
The acid phosphatase protects the sperm from the acidic environment of the vagina.
3. Cowper’s glands:
Cowper’s glands are also known as bulbourethral glands. These are pea-sized and lie on either side of membranous urethra. They secrete a viscous, alkaline, mucous like fluid which acts as a lubricant during copulation.
Semen: It is the viscous, alkaline and milky fluid (pH 7.2 to 7.7) ejaculated by the male reproductive system. Generally, 2.5 to 4.0 ml of semen is given out during a single ejaculation and it contains about 400 million sperms. Semen contains secretion of the epididymis and the accessory glands for nourishing (fructose), neutralizing acidity (Ca++, bicarbonates), activation for movement (prostaglandins).
iii. External genitalia:
a. Penis:
The penis is the male copulatory organ. It is cylindrical and muscular with three bundles of erectile tissue: a pair of postero-lateral tissue called corpora cavernosa and a median corpus spongiosum. The swollen tip of the penis is called glans penis. It is covered by a loose fold of skin called foreskin or prepuce.
b. Scrotum:
It is a loose pouch of pigmented skin lying behind the penis and is divided into a right and left scrotal sac by a septum of tunica dartos made of smooth muscle fibres. The foetal testes are guided into and retained in the scrotum by a short fibro muscular band called gubernaculum. The testes remain suspended in scrotum by a spermatic chord.
The failure of the testis to descend into the scrotum is called cryptorchidism which also results in sterility.
The cremaster and dartos muscles of scrotum help in drawing testes close or away from the body. This helps in maintaining the temperature of the testis 2-3 0C lower than the normal body temperature, necessary for spermatogenesis.
Long answer question.
Describe female reproductive system of human.
Answer:
The human female reproductive system consists of:
i. Internal genitalia:
It includes ovaries, oviducts, uterus, vagina.
a. Ovary:
It is the primary female sex organ. It is a solid, oval, or almond-shaped organ. It is 3 cm in length, 1.5 cm in breadth, and 1 cm thick. It is located in the upper lateral part of the pelvis near the kidneys. Each ovary is held in position by ligaments by attaching it to the uterus and the abdominal wall. The largest of these is the broad ligament formed by a fold of peritoneum. It holds the ovary, oviduct and the uterus to the dorsal body wall. The ovarian ligament attaches the ovary to the uterus.
Functions:
Its main function is production of egg or ovum and the female reproductive hormones.
The ovary produces five hormones viz. estrogen, progesterone, relaxin, activin and inhibin.
b. Oviduct / Fallopian tube / Uterine tube:
These are a pair of muscular ducts lying horizontally over the peritoneal cavity. The proximal part of the tube lies close to the ovary and distally it opens into the uterus. Each tube is 10 to 12 cm in length. It is internally lined by ciliated epithelium. It can be divided into three regions:
1. Infundibulum:
The proximal funnel like the part with an opening called ostium surrounded by many finger-like processes called fimbriae (of these at least one is long and connected to the ovary). The cilia and the movement of fimbriae help in transporting the ovulated egg to the ostium.
2. Ampulla:
It is the middle, long and straight part of the oviduct. Fertilization of the ovum takes place in this region.
3. Isthmus / Cornua:
The distal narrow part of the duct opening into the uterus.
Functions:
Fallopian tubes carry the released egg from the ovary to the uterus. Ampulla provides the site for fertilization of the ovum.
c. Uterus:
It is commonly also called as the womb.
It is a hollow, muscular, pear-shaped organ, located above and behind the urinary bladder. It is about 7.5 cm long, 5 cm broad and 2.5 cm thick. Internally the uterine wall can be distinguished into three layers: The outermost perimetrium, middle thick muscular myometrium, made up of thick layer of smooth muscles. Vigorous contractions of these muscles cause labour during parturition (childbirth). The innermost layer called endometrium or mucosal membrane is made up of stratified epithelium. The thickness of this layer regularly undergoes changes during the menstrual cycle. It is richly supplied with blood vessels and uterine glands. These provide nourishment to the developing foetus.
The uterus can be divided into three regions:
1. Fundus: It is the upper dome shaped part. Normally implantation of the embryo occurs in the fundus.
2. Body: It is the broad part of the uterus which gradually tapers downwards.
3. Cervix: It is the narrow neck about 2.5 cm in length. It extends into the vagina. Its passage has two openings: an internal os/ orifice towards the body, and an external os/ orifice towards the vagina.
Functions:
Uterus receives the ovum. It provides site for implantation, gestation and parturition. It forms placenta for the development of foetus.
d. Vagina:
It is a tubular, female copulatory organ, 7 to 9 cm in length.
It lies between the cervix and the vestibule.
The vaginal wall has an inner mucosal lining, the middle muscular layer and an outer adventitia layer.
The mucosal epithelium is stratified and non-keratinized and stores glycogen.
There are no glands but the cervical secretion of mucus is received in the vagina.
The opening of the vagina into the vestibule is called vaginal orifice. The vaginal orifice is partially covered by the hymen.
Functions:
The vagina acts as a passage for menstrual flow as well as a birth canal during parturition.
ii. External genitalia (Vulva):
The external genital organs of female include parts external to the vagina, collectively called vulva (covering or wrapping), or pudendum. They include the following parts:
a. Vestibule:
It is a median vertical depression of vulva enclosing the urethral and vaginal opening.
b. Labia minora:
These are another pair of thin folds inner to the labia majora with which they merge posteriorly to form the fourchette (frenulum), while towards anterior end they converge into a hood-like covering around the clitoris.
c. Clitoris:
A small conical and sensitive projection lying at the anterior end of labia minora. It has a pair of erectile tissue i.e. corpora cavernosa which is homologous to the penis.
d. Labia majora:
These are a pair of fleshy folds of skin forming the boundary of the vulva. They are homologous to the scrotum. They surround and protect the other parts of the external genitalia and enclose the urethral and vaginal openings in the vestibule.
e. Mons pubis:
It is a fleshy elevation above the labia majora. The Mons pubis and outer part of labia majora show pubic hair.
iii. Accessory glands:
a. Vestibular glands / Bartholin’s glands:
It is a pair of glands homologous to the Bulbourethral or Cowper’s glands of the male. They open into the vestibule and release a lubricating fluid.
b. Mammary glands:
These are accessory organs of the female reproductive system for production and release of milk after parturition. The development of the mammary glands occur at puberty under the influence of estrogen and progesterone. Lactotropic hormone (LTH) or prolactin helps in the development of lactiferous tubules during pregnancy. The mammary glands are a pair of rounded structures present in the subcutaneous tissue of the anterior thorax in the pectoral region (from 2nd to 6th rib). These are modified sweat glands. Each mammary gland contains fatty connective tissue and numerous lactiferous ducts. The glandular tissue of each breast is divided into 15-20 irregularly shaped mammary lobes, each with alveolar glands and lactiferous duct.
Alveolar glands secrete milk which is stored in the lumen of alveoli. The alveoli open into mammary tubules. The tubules of each lobe join to form a mammary duct.
Many mammary ducts join to form a wider mammary ampulla, which is connected to lactiferous duct. These converge towards the nipple located near the tip of the breast.
It is surrounded by a dark brown coloured and circular area of the skin called areola.
Describe the process of fertilization.
Answer:
Fertilization is the process which involves the fusion of the haploid male and female gametes resulting in the formation of a diploid zygote (2n). The process of fertilization is internal and it usually takes place in the ampulla of the fallopian/uterine tube. The fertilized egg or zygote further develops into an embryo within the uterus.
The mechanism of fertilization is as follows:
i. Movement of sperm towards egg:
The ejaculated semen is made up of sperms and some other secretions. This coagulated semen undergoes liquefication and sperms become active. Once the sperms reach the vagina around 50% sperms are demobilized/broken/destroyed and the remaining sperms undergo capacitation.
Capacitation:
Capacitation generally requires 5-6 hours during which the acrosome membrane becomes thin, Ca++ enters the sperm, and sperm tails begin to show rapid whiplash movements. As a result of capacitation, sperms become extra active and begin to start moving upwards from the vagina to the uterus and to the oviducts. Prostaglandins activate the sperms. The vestibular secretions of the female also enhance sperms' motility. The sperms swim at an average speed of 1.5 to 3.0 mm/min and reach the ampulla. The contraction of the uterus and fallopian tubes stimulated by oxytocin of females also aids in the movement of sperm. After capacitation, the sperms may reach the ampulla within 5 minutes.
ii. Entry of sperm into the egg:
Out of 200 to 400 million sperms, only few hundred manage to reach the ampulla, out of which only a single sperm fertilizes the ovum. After the sperm reaches the egg/ovum, its acrosome releases lysins: hyaluronidase and corona penetrating enzymes. These enzymes separate and dissolve the cells of corona radiata, so that the sperm head can pass through the zona pellucida of the egg. The zona pellucida has fertilizin receptor proteins (ZP3, ZP2). The fertilizin binds to specific acid protein- anti-fertilizin of sperm and brings about the attraction of sperms to the egg to enhance fertilization.
Acrosome reaction:
As the sperm head touches the zona pellucida in the animal pole region, its acrosome covering ruptures to release lytic enzymes, acrosin or zona lysin which act on the zona pellucida at the point of contact. This causes egg reaction during which a small fertilization cone/cone of reception is formed on the egg membrane. The sperm head comes in contact with this cone. It results in the production of a weak wave of depolarization. The plasma membrane of both cells dissolves at the point of contact.
The sperm nucleus and the centrioles enter the egg, while other parts remain outside.
As soon as the sperm head touches the vitelline membrane, a cortical reaction gets activated changing the vitelline membrane into a fertilization membrane by deactivating the sperm receptors of zona pellucida.
A distinct perivitelline space is created around the fertilization membrane.
This prevents any further entry of other sperms into the egg i.e. polyspermy is avoided.
iii. Activation of ovum:
The ovum before fertilization was at metaphase II stage. After the contact of sperm head to the vitelline membrane of egg, it gets activated to resume and complete meiosis II. After meiosis II, the second polar body is formed. The germinal vesicle organizes into female pronucleus also known as the true ovum or egg.
The fusion of egg and sperm:
The coverings of male and female pronuclei degenerate, allowing the chromosomal pairing. This results in the formation of a synkaryon by the process called syngamy or karyogamy. The zygote is thus formed. The proximal centriole received from the sperm helps in the formation of the synkaryon spindle and cleavage of the cell into two blastomeres.
The zygote is thus formed.
The proximal centriole received from the sperm helps in the formation of the synkaryon spindle and cleavage of the cell into two blastomeres.
Explain the process by which zygote divides and re-divides to form the morula.
Answer:
The zygote formed as a result of syngamy is activated to divide.
1. Cleavage:
Cleavage is the process of early mitotic division of the zygote into a hollow multicellular blastula. It does not involve the growth of the daughter cells. The cells formed by cleavage are called blastomeres. Since there is no growth phase between the cleavages, the size of blastomeres will be reduced with every successive cleavage.
As the size reduces, the metabolic rate increases. Subsequent cleavages are thus faster than earlier ones. This requires rapid replication of DNA and high consumption of oxygen.
2. Process of cleavage:
In human, cleavage is holoblastic i.e. the whole zygote gets divided. The cleavage planes may be longitudinal or meridional and equatorial or horizontal. It is radial and indeterminate i.e. fate of each blastomere is not predetermined.
The 1st cleavage in the zygote is meridional and occurs at about 30 hours after fertilization.
It divides longitudinally into two blastomeres, one slightly larger than the other.
The 2nd cleavage is also longitudinal but at the right angle to the 1st one and occurs after 30 hours of 1st cleavage.
The 3rd cleavage is horizontal. After 3rd cleavage, the embryo is in the 8-cell stage.
While the cleavages occur, the young embryo is gradually being pushed towards the uterus.
By the end of 4th day after fertilization, the embryo is a solid ball of 16-32 cells and externally looking like mulberry. This stage is thus called a morula.
3. Morula:
The morula shows cells of two types:
a. smaller, clearer cells towards the outer side
b. inner cell mass of larger cells.
Cells are compactly arranged. Till the formation of morula, the zona pellucida is retained around the embryo and thus, there is no change in the overall size from zygote to morula. The morula reaches the isthmus and gains entry into the uterus by the end of day 4.
Biology 12th Standard
Balbharati Solutions for Biology 12th Standard HSC Maharashtra State Board Chapterwise List - Free
Chapter 1: Reproduction in Lower and Higher Plants
Chapter 2: Reproduction in Lower and Higher Animals
Chapter 3: Inheritance and Variation
Chapter 4: Molecular Basis of Inheritance
Chapter 5: Origin and Evolution of Life
Chapter 6: Plant Water Relation
Chapter 7: Plant Growth and Mineral Nutrition
Chapter 8: Respiration and Circulation
Chapter 9: Control and Coordination
Chapter 10: Human Health and Diseases
Chapter 11: Enhancement of Food Production
Chapter 13: Organisms and Populations
Chapter 14: Ecosystems and Energy Flow
Chapter 15: Biodiversity, Conservation and Environmental Issues
Board Paper With Solutions
MARCH 2013, OCTOBER 2013, MARCH 2014, OCTOBER 2014, MARCH 2015, JULY 2015, MARCH 2016, JULY 2016. MARCH 2017, JULY 2017